Delivering value and affordability to consumers
Express Scripts saves consumers money.
A prescription doesn't work if it is priced out of reach for consumers
Express Scripts relentlessly advocates on behalf of our clients and their members to make lifesaving therapies and medications more affordable. Navigating the health care system can be hard. Express Scripts simplifies access to the most clinically effective medications and helps people stay on them—to help prevent disease progression and costly downstream interventions.

Real-Time Prescription Benefit Tool
Express Scripts creates unique programs, such as the Real-Time Prescription Benefit Tool that allows providers and customers to see if a medication is covered, how much it will cost, whether home delivery is available, and, if searching for a brand name drug, see the costs for any generic or biosimilar medications.
Express Scripts enrolled members enrolled pay:
<$15
per prescription when enrolled in Commercial health plans
<$9
per prescription with Medicare prescription drug coverage
<$1
per prescription with Medicaid prescription drug coverage2
Express Scripts offers value-based solutions that can help chronic conditions
Express Scripts’ SafeGuardRx program seeks to address this issue through a suite of solutions across eleven complex and costly disease states, including oncology, inflammatory conditions, multiple sclerosis and other conditions.
Specifically, SafeGuardRx provides proactive medication adherence monitoring and condition-specific coaching services to customers. Through this program, Express Scripts pharmacists are available to talk through topics such as: medication options, side effects, barriers to medication adherence and possible interactions.

As a result of SafeGuardRx, clients and consumers have seen not only substantial savings, but also higher therapy completion rates and improved clinical outcomes:
As a result of SafeGuardRx, clients and consumers have seen not only substantial savings, but also higher therapy completion rates and improved clinical outcomes:
16%
higher adherence across all programs when compared to the industry average for patients with chronic illness.5
31%
increase in the number of patients filling their prescription within 30 days in 20236
81%
of consumers enrolled in our digital solutions lost an average of 3.6% of their body weight through our digital tools.5
$388M
paid directly to SafeGuardRx clients—the highest value yet!7
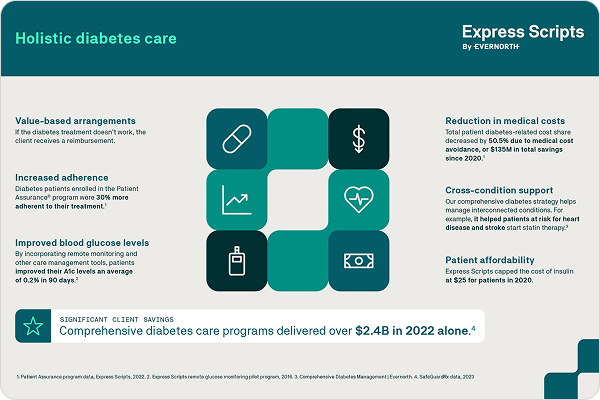
Lowering the cost of diabetes care and insulin
For people living with diabetes, the high list price of insulin and other diabetes drugs has the potential to create financial burdens. At Express Scripts, it is our job to support access to safe treatments at a cost patients and employers can afford, so we got to work. Since 2020, Express Scripts has been proud to cap patient out-of-pocket costs for these drugs at $25 for up to a 34-day supply (or $75 for a 90-day supply) for the over 11 million members enrolled in our Patient Assurance Program.
By bringing manufacturers to the table around the common goal of an affordable, predictable patient experience, the Patient Assurance Program has delivered more than $225 million in patient savings for insulin and other diabetes medications since its launch.8

We haven’t stopped at insulin.
Because diabetes management doesn’t always require insulin, particularly for Type 2 diabetes, our Patient Assurance Program (PAP) has expanded to include non-insulin diabetes treatments, such as DPP-4 inhibitors, GLP-1 agonists, and SGLT2 inhibitors, capping out of pocket costs at $25 for up to a 34-day supply.

By capping the cost of diabetes medications—thereby addressing cost as a barrier to care—the PAP has significantly improved adherence and patient clinical outcomes.
In 2024 about 77% of Express Scripts members pay $25 or less for their insulin at the pharmacy counter – either through the Patient Assurance Program or their plan’s benefit design. 97% pay less than $35 copay for their insulin medications.8
For patients, their total diabetes-related cost share—inclusive of medical and pharmacy costs—decreased by 50.5% since 2020.9
According to Evernorth data in 2023, medical cost savings for plan sponsors totaled $248+ million due to increased diabetes adherence and improved outcomes.10
In 2023, the Patient Assurance Program helped close to 400K patients with affordable diabetes medications which resulted in close to $138M in prescription cost savings and an estimated $600M in medical cost avoidance savings.10
A look at diabetes
For patients with diabetes, Express Scripts has worked to address costs for insulin, including the Patient Assurance Program where patients spend no more than $25 for a 30-day supply—well before government regulations and recent insulin manufacturer moves.
Consumers taking insulin saved more than $18 million with point-of-sale discounts in 2022 alone, part of more than $45 million in member savings on insulin since the program launched.11
$18M as saved by consumers taking insulin through point-of-sale discounts
Contributing to over $45 million in total member savings on insulin since the program's launch, in 202211
On average, members in plans that use Express Scripts only pay $22.78 for a 30-day supply of insulin, either through our Patient Assurance Program, their plan sponsor’s benefit design, or both.8
Semglee, the first interchangeable biosimilar insulin, was preferred on the Express Scripts National Preferred Formulary in 2022—resulting in ~$20 million in savings for clients and customers10
Express Scripts helps improve population health, reduce waste and increase medication adherence
Express Scripts processes more than one billion pharmacy claims annually, helping people live their healthiest lives.12 We harness real-time data, insights, and care management programs, such as patient and provider interactions, to help patients start and stay on the most effective treatments.
Studies show that approximately one percent of pharmacy costs are attributable to fraud, waste, and abuse, amounting to billions of dollars in unnecessary costs.13 Express Scripts uses drug utilization reviews to reduce waste and helps ensure the prescribed medication is appropriate for the individual patient.14
Sources
- Visante estimates for 2022 based on data from multiple sources, including CMS National Health Expenditures, Drug Channels and IQVIA.
- Averages based on Express Scripts entire book of business
- Watanabe JH, McInnis T, Hirsch JD. “Cost of Prescription Drug-Related Morbidity and Mortality” Ann Pharmacother. 2018
- CDC, “Chronic Disease Prevalence in the US: Sociodemographic and Geographic Variations by Zip Code Tabulation Area”
- 2023 Evernorth data
- 2024 Evernorth data
- 2023 SafeGuardRx data
- Express Scripts. Patient Assurance Program data. 2024.
- 2022 Evernorth data
- Express Scripts. Internal Data. 2024
- Affordable Cost of Diabetes Medication Can Improve Health Outcomes June 15, 2022
- Evernorth, “How PBMs streamline the patient experience”
- AMCP: Fraud, waste, and abuse in prescription drug benefits.
- Evernorth, What Is Drug Trend and How to Manage it April 20, 2022